- Visiting Hours: Mon-Sat / 8:00 AM - 8:00 PM
- Visiting Hours: Mon-Sat / 8:00 AM - 8:00 PM
Type 1 diabetes occurs when the endo pancreas is unable to produce insulin, the hormone responsible for processing and storage of sugar from our diet. Type 1 diabetes is often diagnosed in childhood or adolescence but can occur at any point. The following are some primary symptoms that present in children, adolescents and adults that can help a doctor or clinician diagnose the disease:
It is important to note that not every person with Type 1 diabetes will have all of these symptoms and do not have to experience them at the same time. The onset of symptoms depends on the level of disease progression and varies from person to person. Type 1 diabetes has genetic links and runs in the family; so, if someone has a close relative (father/mother) with diabetes, then, there are good chances they will get it as well. It’s important to note that symptoms present themselves faster in Type 1 diabetes because the body is unable to produce insulin properly, affecting blood glucose levels sharply.





Type 2 diabetes is typically an adult-onset disease (middle-aged people are more likely to get it) and is a result of the body either not having enough insulin or being unable to properly use the insulin to store sugar, termed as insulin resistance. Symptoms typically appear at later stages in life and are common in those aged 35-45. As Type 2 diabetes results from the body’s inability to use insulin properly, the symptoms appear more gradually and may not be noticed. Some commonly experienced symptoms are:
Any or all of these symptoms may be seen in individuals with diabetes and may present in any order. Diabetes, whether it is Type 1 or 2, is a lifelong condition and will need regular treatment and monitoring.



Gestational diabetes (GDM), as the term suggests, is seen only in pregnant women. A small percentage of pregnant women (2-10%) develop insulin resistance that leads to diabetes. In India, that percentage is higher than in Western countries at 10-14%. Not all expectant mothers will get gestational diabetes, but some have a high risk of developing the condition. Women who are overweight, have a BMI of over 30, have had GDM in a previous pregnancy, or are over the age of 40 are all at greater risk of getting diabetes while pregnant.
Gestational diabetes often does not show any symptoms and is diagnosed when a routine blood sugar test is performed on expecting mothers. However, some commonly seen symptoms are:
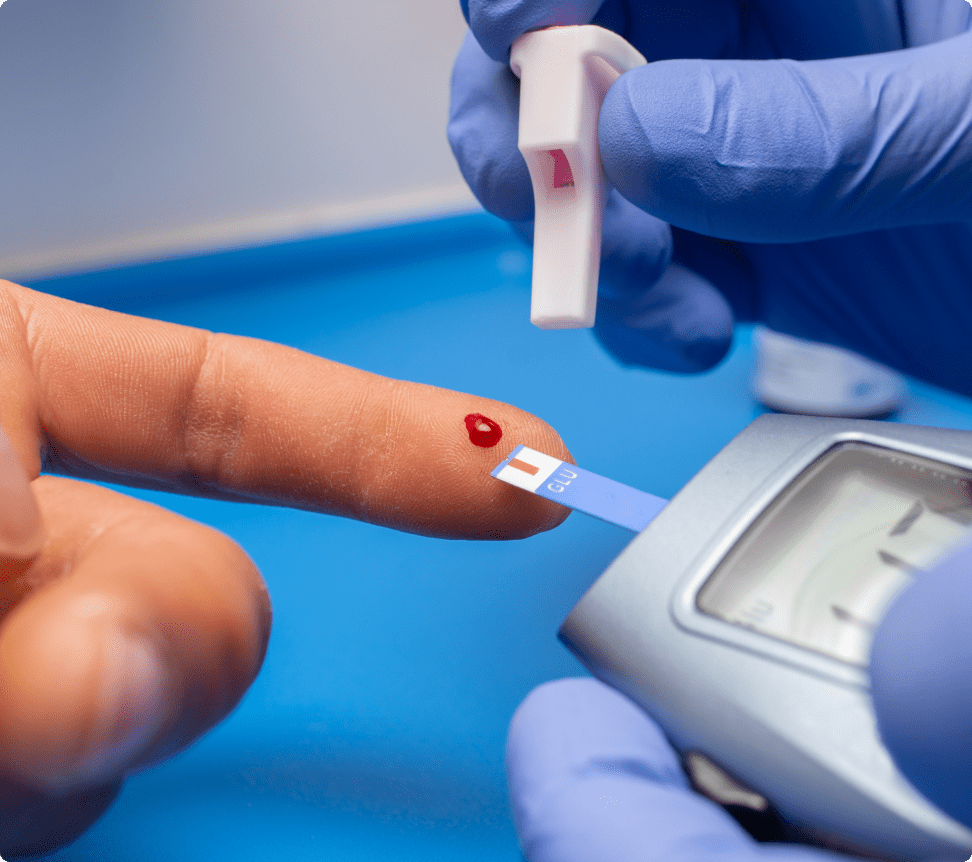
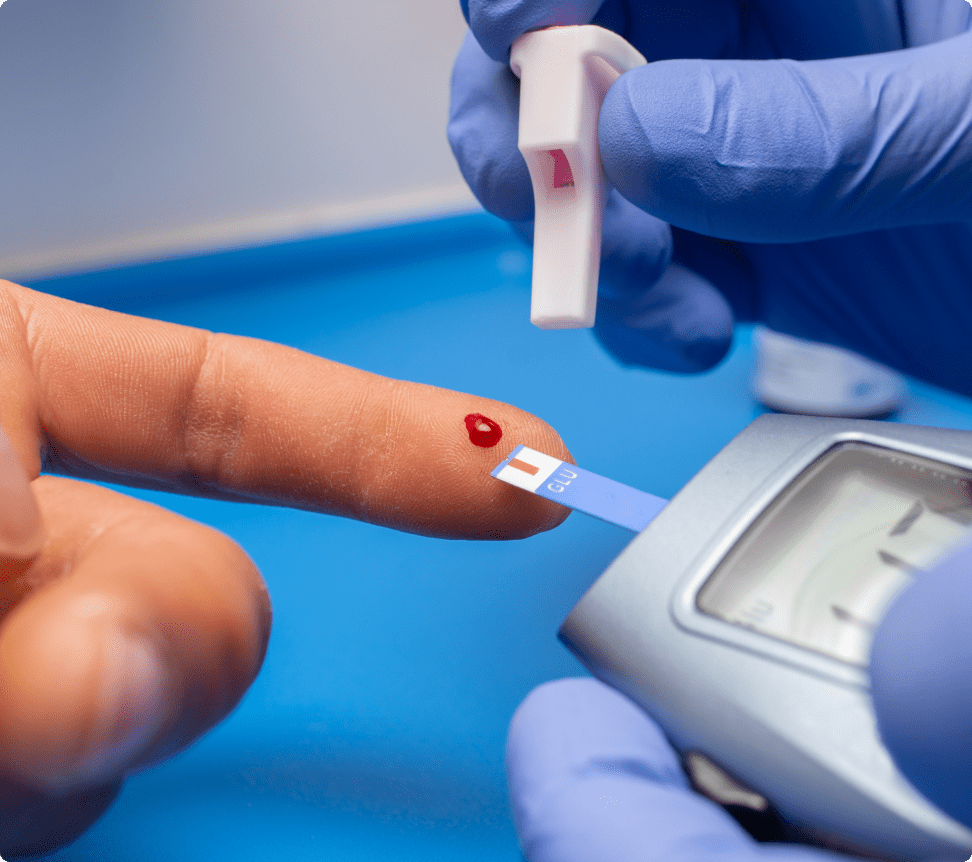
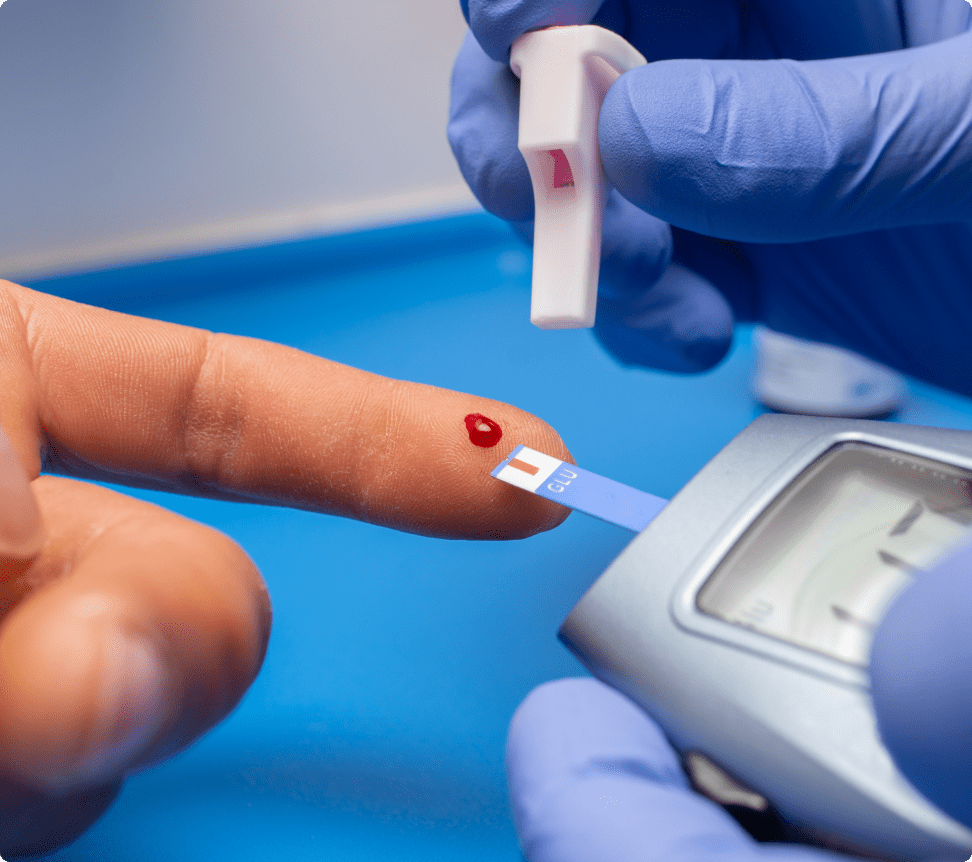
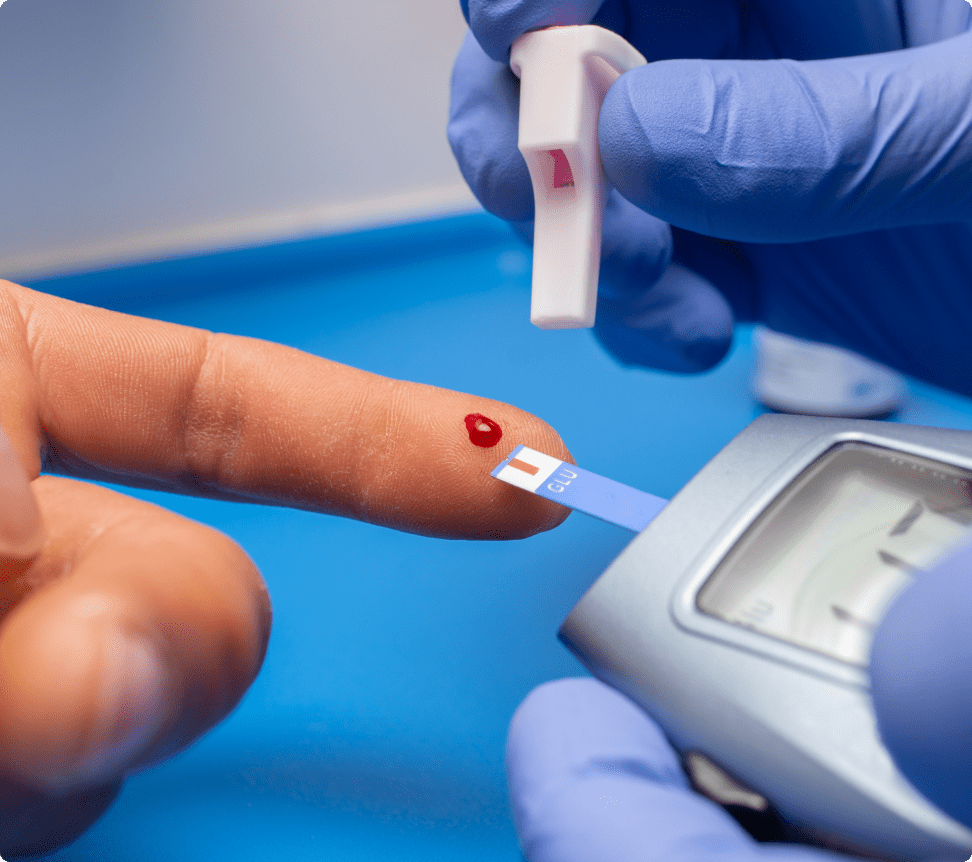
All these are symptoms that can occur commonly during a pregnancy and are not unique to diabetes. The definitive diagnostic method for GDM is a blood sugar test. If the values of blood samples taken before and after food are higher than normal, they indicate that the woman has diabetes and will need monitoring and medications to control it throughout the pregnancy. In India, every expecting mother is given an Oral Glucose Challenge test (OGCT) every trimester. If the sugar value is above 140 mg/dL even once, they are monitored thoroughly to ensure both the mother and the baby are safe.


It can be hard to decide about consulting a doctor when diabetes is suspected. Getting a positive diagnosis can be mentally and financially draining, so a large number of people tend to put it off. But, diabetes is a lifelong disease and has to be dealt with sooner than later. A family history of diabetes is a primary factor to consult a doctor, as the chances of a person who has relatives with diabetes getting the disease themselves is very high.
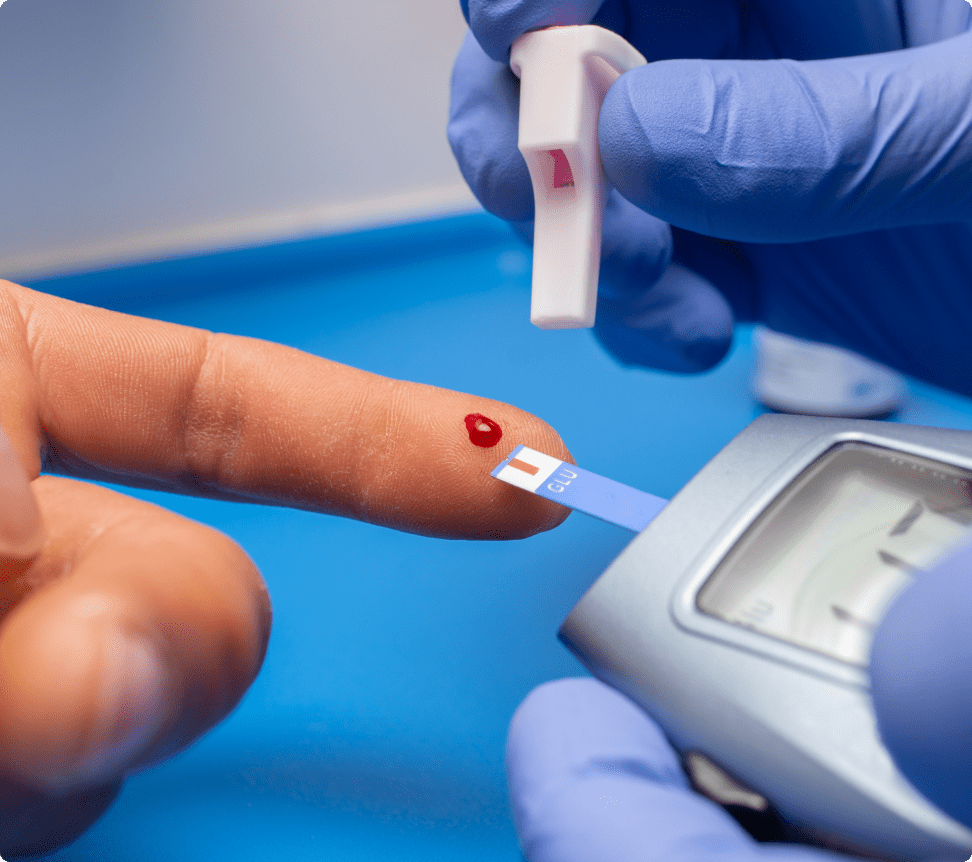
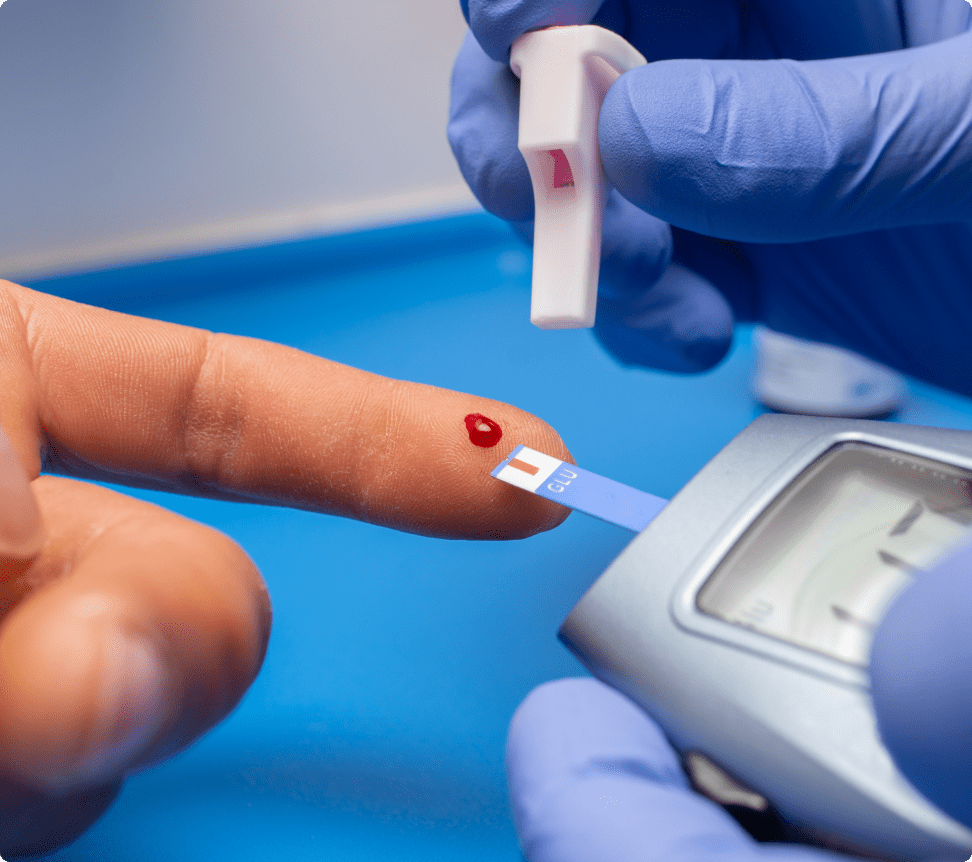
It is recommended to monitor blood sugar regularly, either at home or a lab. A high blood sugar level can indicate that you are prediabetic. In a clinical setting, diabetes is screened for using the values of HbA1C (glycated haemoglobin). When the value is above normal, it indicates the person is diabetic and needs to get some form of treatment and continue monitoring their sugar levels. These days, there are at-home monitoring devices for checking blood sugar levels; bi-annual scans are recommended too.
Knowing the risk factors for a disease can help us understand what we can do to avoid getting it. The primary risk factor for diabetes is a family history of the disease. So, if someone has close relatives with diabetes and several generations of family who have had the disease, then, chances are they will get it too. Genetics and family history are non-modifiable risk factors (cannot be controlled or reduced), but some modifiable risk factors for diabetes are:


Prevention is always better than cure. We perform routine physical and wellness check-ups to ensure that any disease is detected and treated in its initial stages.
Complications of diabetes can be of two kinds, the acute ones occurring at any time and the chronic complications that present slowly over a longer period.
People with diabetes must be alert and monitor themselves regularly. Most complications of diabetes occur with a late diagnosis, failing to follow the treatment regimen and not having a proper diet and exercise. If the prescribed medication and other lifestyle modifications are followed properly, an individual with diabetes can prevent the complications.
Insulin is a hormone that helps in regulating glucose in the bloodstream and is secreted by specialized pancreatic cells. The stomach breaks down the carbohydrates in the food we eat into glucose, which is then released into the bloodstream. Our cells use this glucose for energy to carry out all body functions. Without insulin, cells cannot access the glucose for energy, and the body turns to other sources such as proteins and fats to meet the demand.
When there is a rise in the blood glucose levels, the pancreas releases insulin to help move the sugar into cells for use or storage. When the level of sugar in the blood falls, the insulin level also drops. Thus, insulin plays a crucial role in helping move glucose from the blood to the cells, organs and tissues that need it. If insulin is not secreted in sufficient quantities or does not function as normal, the condition results in diabetes.
Glucose is produced when the body breaks up complex carbohydrates such as starch, rice, wheat, etc., down to the most basic chemical unit. The word ‘glucose’ is often used interchangeably with sugar, essentially referring to a building block of all carbohydrates. Our body breaks down the carbohydrates in food into glucose and releases it into the blood to be used by cells and tissues for carrying out all essential functions.
Glucose is the most abundant and used source of energy by cells to carry out all the bodily functions that keep us alive and well. In a series of chemical reactions, glucose is broken down by cells into energy units or ATPs, which are then consumed by the body for activities such as walking, running, thinking, reading, etc. A healthy and active person will have sufficient levels of glucose consumed through their diet.
Would you like to manage your diabetes better and lead a healthier, normal life?
Take an appointment with our senior diabetologist today!